GIVE NOW before 2025 ends—your gift will be doubled to help children in need. Click here to 2x your impact!

Ranked nationally in pediatric care.
Arkansas Children's provides right-sized care for your child. U.S. News & World Report has ranked Arkansas Children's in seven specialties for 2025-2026.

It's easier than ever to sign up for MyChart.
Sign up online to quickly and easily manage your child's medical information and connect with us whenever you need.

We're focused on improving child health through exceptional patient care, groundbreaking research, continuing education, and outreach and prevention.

When it comes to your child, every emergency is a big deal.
Our ERs are staffed 24/7 with doctors, nurses and staff who know kids best – all trained to deliver right-sized care for your child in a safe environment.

Arkansas Children's provides right-sized care for your child. U.S. News & World Report has ranked Arkansas Children's in seven specialties for 2025-2026.

Looking for resources for your family?
Find health tips, patient stories, and news you can use to champion children.

Support from the comfort of your home.
Our flu resources and education information help parents and families provide effective care at home.

Children are at the center of everything we do.
We are dedicated to caring for children, allowing us to uniquely shape the landscape of pediatric care in Arkansas.

Transforming discovery to care.
Our researchers are driven by their limitless curiosity to discover new and better ways to make these children better today and healthier tomorrow.

We're focused on improving child health through exceptional patient care, groundbreaking research, continuing education, and outreach and prevention.

Then we're looking for you! Work at a place where you can change lives...including your own.

When you give to Arkansas Children's, you help deliver on our promise of a better today and a healthier tomorrow for the children of Arkansas and beyond

Become a volunteer at Arkansas Children's.
The gift of time is one of the most precious gifts you can give. You can make a difference in the life of a sick child.

Join our Grassroots Organization
Support and participate in this advocacy effort on behalf of Arkansas’ youth and our organization.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

When you give to Arkansas Children’s, you help deliver on our promise of a better today and a healthier tomorrow for the children of Arkansas and beyond.

Your volunteer efforts are very important to Arkansas Children's. Consider additional ways to help our patients and families.

Join one of our volunteer groups.
There are many ways to get involved to champion children statewide.

Make a positive impact on children through philanthropy.
The generosity of our supporters allows Arkansas Children's to deliver on our promise of making children better today and a healthier tomorrow.

Read and watch heart-warming, inspirational stories from the patients of Arkansas Children’s.

Hello.

Arkansas Children's Hospital
General Information 501-364-1100
Arkansas Children's Northwest
General Information 479-725-6800
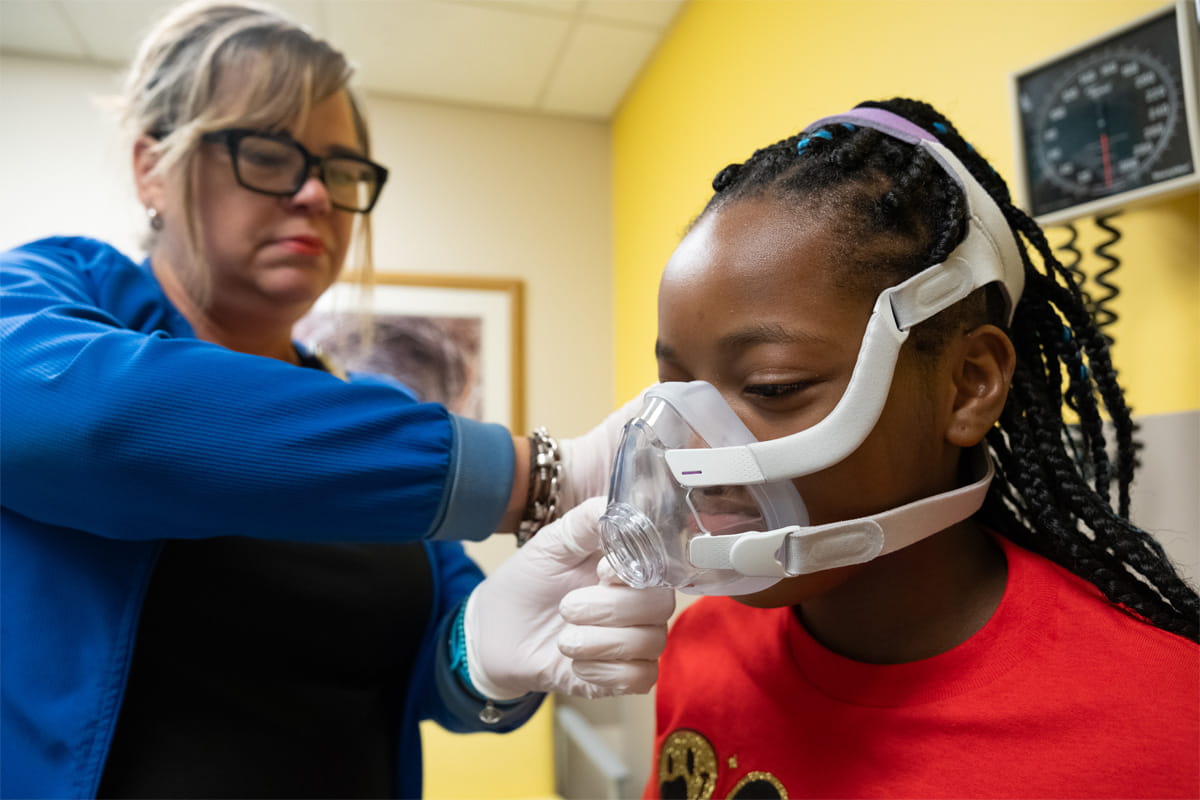
Pulmonary
The Pulmonary Clinic at Arkansas Children’s provides infants and children with complete diagnosis and treatment of acute and chronic lung disease. It is the only Cystic Fibrosis Center in the state reviewed and approved by the national Cystic Fibrosis Foundation.

Possible Treatments
Pulmonary function tests are a series of tests, which evaluate how well your lungs are performing.
Staffed by Licensed Respiratory Care Practitioners, pulmonary performs many tests that help physicians evaluate a patient’s lung health. “Pulmonary function tests”, usually called PFT’s are the most frequently ordered pulmonary lab tests. Different types of PFT’s can be performed depending on the age of the child. Each test requires a certain level of cooperation for the test to be successful and accurate. Generally, PFT’s are ordered within the following guidelines:
- Ages 8 and older: Spirometry every visit, lung volumes as needed
- Ages 6 & 7: Spirometry each visit
- Ages 3, 4 and 5: Spirometry as able (many this age cannot correctly perform test)
- Ages up to 3: Infant pulmonary function testing
Infant Pulmonary Function testing is done in the main pulmonary lab. When patients are old enough to cooperate, they will be testing in either the pulmonary lab located on the second floor in the main hospital or the satellite pulmonary lab.
State-of-the-Art Lung Function Tests
Pulmonary function tests, called PFTs, are tests that see how well your lungs work. They are the most often ordered pulmonary lab tests. Our Pulmonary Clinic is staffed by Licensed Respiratory Care Practitioners and performs many tests to help physicians check a patient’s lung health. To accurately diagnose and treat lung conditions in children, we offer pulmonary function tests.
Diagnostic Tests
Body Plethysmography
Bronchoscopy
Cold Air Challenge
Cough Peak Flow
Diffusion Capacity
Exercise-induced Bronchoconstriction Study
Helium Dilution
Lung Volumes
Maximum Expiratory Pressure
Maximum Inspiratory Pressure
Pre-Post Bronchodilator Study
Six Minute Walk Test
Spirometry and Bronchodilator Response
Sweat Testing
-
 Hospital Services
Hospital ServicesSend an E-card
Bookmark Send an E-cardBrighten the day of the patient by sending a word of encouragement.
-
 Hospital Services
Hospital ServicesChild Life
Bookmark Child LifeChild Life reduces stress and promotes positive coping using developmentally appropriate preparation, education, and play at Arkansas Children's.
-
 Amenities
AmenitiesHospital Amenities
Bookmark Hospital AmenitiesArkansas Children's offers on-site dining, shuttle services, and gift shops, as well as discounted hotels and RV parks nearby.
 Conditions
Jump to
Overview
Conditions
Treatments
Health at Home
Conditions
Jump to
Overview
Conditions
Treatments
Health at Home
Possible Treatments
Pulmonary function tests are a series of tests, which evaluate how well your lungs are performing.
Staffed by Licensed Respiratory Care Practitioners, pulmonary performs many tests that help physicians evaluate a patient’s lung health. “Pulmonary function tests”, usually called PFT’s are the most frequently ordered pulmonary lab tests. Different types of PFT’s can be performed depending on the age of the child. Each test requires a certain level of cooperation for the test to be successful and accurate. Generally, PFT’s are ordered within the following guidelines:
- Ages 8 and older: Spirometry every visit, lung volumes as needed
- Ages 6 & 7: Spirometry each visit
- Ages 3, 4 and 5: Spirometry as able (many this age cannot correctly perform test)
- Ages up to 3: Infant pulmonary function testing
Infant Pulmonary Function testing is done in the main pulmonary lab. When patients are old enough to cooperate, they will be testing in either the pulmonary lab located on the second floor in the main hospital or the satellite pulmonary lab.
State-of-the-Art Lung Function Tests
Pulmonary function tests, called PFTs, are tests that see how well your lungs work. They are the most often ordered pulmonary lab tests. Our Pulmonary Clinic is staffed by Licensed Respiratory Care Practitioners and performs many tests to help physicians check a patient’s lung health. To accurately diagnose and treat lung conditions in children, we offer pulmonary function tests.
Diagnostic Tests
Body Plethysmography
Bronchoscopy
Cold Air Challenge
Cough Peak Flow
Diffusion Capacity
Exercise-induced Bronchoconstriction Study
Helium Dilution
Lung Volumes
Maximum Expiratory Pressure
Maximum Inspiratory Pressure
Pre-Post Bronchodilator Study
Six Minute Walk Test
Spirometry and Bronchodilator Response
Sweat Testing
-
 Hospital Services
Hospital ServicesSend an E-card
Bookmark Send an E-cardBrighten the day of the patient by sending a word of encouragement.
-
 Hospital Services
Hospital ServicesChild Life
Bookmark Child LifeChild Life reduces stress and promotes positive coping using developmentally appropriate preparation, education, and play at Arkansas Children's.
-
 Amenities
AmenitiesHospital Amenities
Bookmark Hospital AmenitiesArkansas Children's offers on-site dining, shuttle services, and gift shops, as well as discounted hotels and RV parks nearby.
 Treatments
Jump to
Overview
Conditions
Treatments
Health at Home
Treatments
Jump to
Overview
Conditions
Treatments
Health at Home
Possible Treatments
Pulmonary function tests are a series of tests, which evaluate how well your lungs are performing.
Staffed by Licensed Respiratory Care Practitioners, pulmonary performs many tests that help physicians evaluate a patient’s lung health. “Pulmonary function tests”, usually called PFT’s are the most frequently ordered pulmonary lab tests. Different types of PFT’s can be performed depending on the age of the child. Each test requires a certain level of cooperation for the test to be successful and accurate. Generally, PFT’s are ordered within the following guidelines:
- Ages 8 and older: Spirometry every visit, lung volumes as needed
- Ages 6 & 7: Spirometry each visit
- Ages 3, 4 and 5: Spirometry as able (many this age cannot correctly perform test)
- Ages up to 3: Infant pulmonary function testing
Infant Pulmonary Function testing is done in the main pulmonary lab. When patients are old enough to cooperate, they will be testing in either the pulmonary lab located on the second floor in the main hospital or the satellite pulmonary lab.
State-of-the-Art Lung Function Tests
Pulmonary function tests, called PFTs, are tests that see how well your lungs work. They are the most often ordered pulmonary lab tests. Our Pulmonary Clinic is staffed by Licensed Respiratory Care Practitioners and performs many tests to help physicians check a patient’s lung health. To accurately diagnose and treat lung conditions in children, we offer pulmonary function tests.
Diagnostic Tests
Body Plethysmography
Bronchoscopy
Cold Air Challenge
Cough Peak Flow
Diffusion Capacity
Exercise-induced Bronchoconstriction Study
Helium Dilution
Lung Volumes
Maximum Expiratory Pressure
Maximum Inspiratory Pressure
Pre-Post Bronchodilator Study
Six Minute Walk Test
Spirometry and Bronchodilator Response
Sweat Testing
-
 Hospital Services
Hospital ServicesSend an E-card
Bookmark Send an E-cardBrighten the day of the patient by sending a word of encouragement.
-
 Hospital Services
Hospital ServicesChild Life
Bookmark Child LifeChild Life reduces stress and promotes positive coping using developmentally appropriate preparation, education, and play at Arkansas Children's.
-
 Amenities
AmenitiesHospital Amenities
Bookmark Hospital AmenitiesArkansas Children's offers on-site dining, shuttle services, and gift shops, as well as discounted hotels and RV parks nearby.
 Health at Home
Jump to
Overview
Conditions
Treatments
Health at Home
Health at Home
Jump to
Overview
Conditions
Treatments
Health at Home
Possible Treatments
Pulmonary function tests are a series of tests, which evaluate how well your lungs are performing.
Staffed by Licensed Respiratory Care Practitioners, pulmonary performs many tests that help physicians evaluate a patient’s lung health. “Pulmonary function tests”, usually called PFT’s are the most frequently ordered pulmonary lab tests. Different types of PFT’s can be performed depending on the age of the child. Each test requires a certain level of cooperation for the test to be successful and accurate. Generally, PFT’s are ordered within the following guidelines:
- Ages 8 and older: Spirometry every visit, lung volumes as needed
- Ages 6 & 7: Spirometry each visit
- Ages 3, 4 and 5: Spirometry as able (many this age cannot correctly perform test)
- Ages up to 3: Infant pulmonary function testing
Infant Pulmonary Function testing is done in the main pulmonary lab. When patients are old enough to cooperate, they will be testing in either the pulmonary lab located on the second floor in the main hospital or the satellite pulmonary lab.
State-of-the-Art Lung Function Tests
Pulmonary function tests, called PFTs, are tests that see how well your lungs work. They are the most often ordered pulmonary lab tests. Our Pulmonary Clinic is staffed by Licensed Respiratory Care Practitioners and performs many tests to help physicians check a patient’s lung health. To accurately diagnose and treat lung conditions in children, we offer pulmonary function tests.
Diagnostic Tests
Body Plethysmography
Bronchoscopy
Cold Air Challenge
Cough Peak Flow
Diffusion Capacity
Exercise-induced Bronchoconstriction Study
Helium Dilution
Lung Volumes
Maximum Expiratory Pressure
Maximum Inspiratory Pressure
Pre-Post Bronchodilator Study
Six Minute Walk Test
Spirometry and Bronchodilator Response
Sweat Testing
-
 Hospital Services
Hospital ServicesSend an E-card
Bookmark Send an E-cardBrighten the day of the patient by sending a word of encouragement.
-
 Hospital Services
Hospital ServicesChild Life
Bookmark Child LifeChild Life reduces stress and promotes positive coping using developmentally appropriate preparation, education, and play at Arkansas Children's.
-
 Amenities
AmenitiesHospital Amenities
Bookmark Hospital AmenitiesArkansas Children's offers on-site dining, shuttle services, and gift shops, as well as discounted hotels and RV parks nearby.
Arkansas Children's MyChart
Manage your child's medical information and connect with your Arkansas Children's medical team anytime online!
Log in to MyChart-
 Hospital Services
Hospital ServicesSend an E-card
Bookmark Send an E-cardBrighten the day of the patient by sending a word of encouragement.
-
 Hospital Services
Hospital ServicesChild Life
Bookmark Child LifeChild Life reduces stress and promotes positive coping using developmentally appropriate preparation, education, and play at Arkansas Children's.
-
 Amenities
AmenitiesHospital Amenities
Bookmark Hospital AmenitiesArkansas Children's offers on-site dining, shuttle services, and gift shops, as well as discounted hotels and RV parks nearby.